A protein that plays a critical role in helping malaria parasites infect red blood cells – known as apical membrane protein 1 (AMA1) – has been found to bind to more than one receptor on the surface of the cells.
The discovery, published this week in Cellular and Molecular Life Sciences, has significant implications for how best to target the protein with vaccines and therapeutics.
Globally, there are over 240 million cases of malaria and over 600,000 deaths due to the disease reported each year, most caused by either the Plasmodium falciparum or the Plasmodium vivax malaria parasites.
Progress in combating malaria has stalled since 2015, emphasising the need for the development of new vaccines and other interventions.
AMA1 is unusual in that it’s one of the few proteins used for infection of red blood cells that is shared by both P. falciparum and P. vivax, which are evolutionarily very distant from each other.
Both cause malaria, but have a lot of important differences in terms of the parasites themselves and the disease they cause.
AMA1 is essential for both these malaria parasites to get into red blood cells, which is why it’s such a good target for malaria vaccines, said Professor James Beeson, head of Burnet Institute’s Malaria Immunity and Vaccines Research Group and senior author on the research.
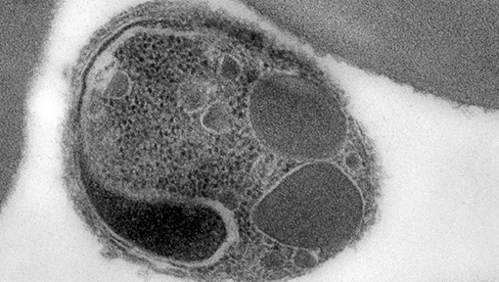
“What AMA1 does is it sticks to a receptor on the surface of the cell, and that enables the malaria parasite to get into the red blood cell,” Professor Beeson said.
“We thought that the protein only had one way of binding to the surface of the cell, but this research revealed that it can also bind to an additional receptor.”
This discovery could explain why vaccines and therapeutics targeting AMA1 have not been successful, Professor Beeson said.
“Uncovering what this other interaction is and targeting it as well might significantly improve our vaccine strategies, which aim to block malaria from infecting red blood cells,” he said.
“Now we’ve got part of the explanation at least, we can take a different approach to designing vaccines that more effectively target the protein and hit it in the right spots.
“And because AMA1 is essential for both P. falciparum and P. vivax, if we can unlock that mystery then we’ve got a strategy for both diseases.”
This could be a ‘two pronged’ response, for example, combining vaccines or therapeutics that target each receptor individually.
The RTS,S vaccine currently being given to young children in Africa to protect against P. falciparum malaria, only has modest protection and doesn’t last very long, Professor Beeson said.
“That’s why identifying these new strategies to fight malaria is so important,” he said.
The work was conducted in collaboration with the University of Adelaide and the Walter Reed Army Institute for Research in the US.
Link to the paper: https://link.springer.com/article/10.1007/s00018-023-04712-z

